Body Composition
(47) DETERMINATION OF LOW ENERGY AVAILABILITY BY DUAL X-RAY ABSORPTIOMETRY VERSUS AIR DISPLACEMENT PLETHYSMOGRAPHY IN COLLEGIATE ATHLETES

Devon Trieschock, MS LAT ATC EMT (she/her/hers)
Graduate Student
George Mason University
Coraopolis, Pennsylvania, United States
Meghan Magee, PhD, CSCS
Graduate Student
George Mason University
Centreville, Virginia, United States
Andrew R. Jagim, PhD
Director of Sports Medicine Research
Mayo Clinic Health System
Holmen, Wisconsin, United States
Jennifer Fields, PhD, CSCS*D, CISSN
Assistant Professor
Springfield College
Springfield, Massachusetts, United States
Margaret Jones
Professor
George Mason University
Fairfax, Virginia, United States
Poster Presenter(s)
Author(s)
Background: Low energy availability (LEA) can lead to decrements in athlete health and sport performance. Determination of fat free mass (FFM) is necessary to calculate EA, and a valid assessment tool is critical to the process. Different instruments may provide varied measurements of FFM, which may lead to differences in calculated EA values. Currently, limited data exist on how instrumentation selection to determine FFM may influence EA status in collegiate team sport athletes.
Purpose: To examine differences in EA values based upon selection of body composition instrumentation selection.
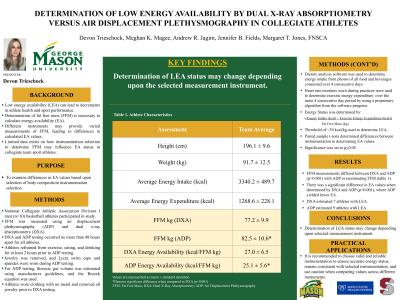
Methods: National Collegiate Athletic Association Division I men’s basketball athletes (n=10) participated. Body composition was evaluated using air displacement plethysmography (ADP) and dual-energy x-ray absorptiometry (DXA). Prior to ADP testing, athletes refrained from exercise, eating, and drinking (except water) for at least 2 hours. Jewelry was removed, and athletes wore spandex and a Lycra swim cap during assessment in accordance with standard operating procedures. Thoracic gas volume was estimated and the Brozek equation was used to determine percent body fat. A DXA scan was completed within 48 hours of ADP testing; athletes removed jewelry and wore clothing without metal. FFM was determined from ADP and DXA. To evaluate EA status, athletes completed a 4-day dietary analysis for determination of energy intake. Photos of all food and beverage consumed were submitted to the research team, and a nutrition software established a 4-day average for energy intake. During the same 4 days, athletes wore a heart rate monitor in training to determine their exercise energy expenditure. Energy availability was calculated as follows: (energy intake – exercise energy expenditure)/FFM (kg). LEA status was determined using the threshold of 30 kcals/kg of FFM. Paired samples t-tests were used to determine differences between instrumentation in establishing EA values. Significance was set to p<u><0.05.
Results: Athlete characteristics are included in Table 1. FFM measurements differed between DXA and ADP (p< 0.001) with ADP overestimating FFM. Further, there was a significant difference in EA values when determined by DXA and ADP (p< 0.001), where DXA yielded greater EA. DXA identified 7 athletes as LEA compared to 9 identified as LEA with ADP.
Conclusion: Determination of LEA status may change depending upon the selected measurement instrument. PRACTICAL APPLICATION: Having accurate measures of FFM is vital to determination of LEA status in athletes. Therefore, it is recommended to choose valid and reliable instrumentation and to remain consistent with the selected instrumentation.
Acknowledgements: None
